Targeted therapies that selectively bind and act through molecules expressed on the surface of cancer cells are a significant advance in cancer treatment because they are more effective and better tolerated than traditional cytotoxic drugs.
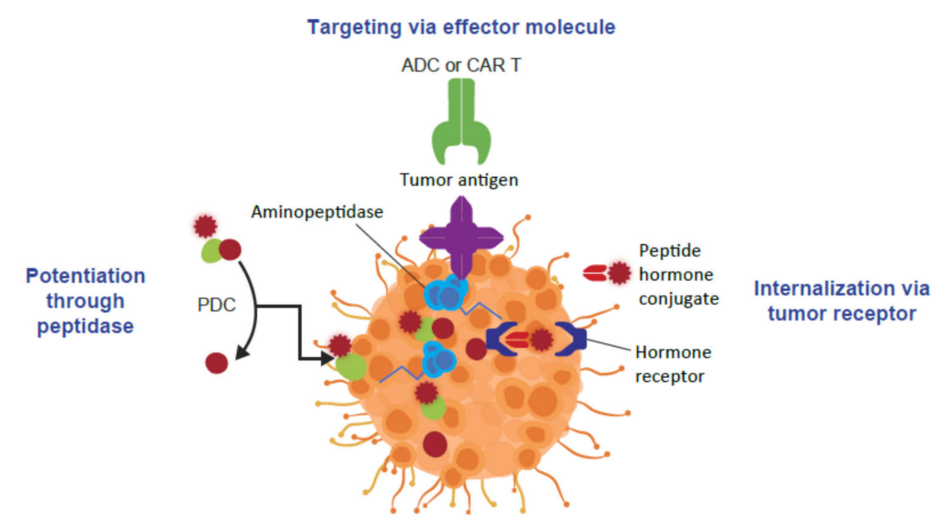
In cancer treatment, there are three targeted approaches used to enhance the specificity and antitumor activity of cancer therapy. Targeted preparations can be designed to inhibit proteins expressed by tumor cells, such as receptors or enzymes; Another approach is to bind effector molecules (e.g., ADC, biantibodies, or CAR-T) to molecules overexpressed on the surface of tumor cells and synergistically inhibit tumor cell division while providing cytotoxic payloads or stimulating tumor-directed immune responses; A third approach is to use peptide-conjugate drugs (PDCs) to drive the enrichment of toxic payloads in tumor cells.
Many of the targeted drugs currently used in clinical practice are based on monoclonal antibodies, however, the therapeutic application of ADCs is limited by their physicochemical and pharmacodynamic properties. PDC's use of peptides as tumor targeting vectors has many advantages, compared to ADCs, they are easy to synthesize, structural modifications can be easily introduced, and support rational drug design to improve bioavailability, affinity, and stability. In addition, peptides have low immunogenicity.
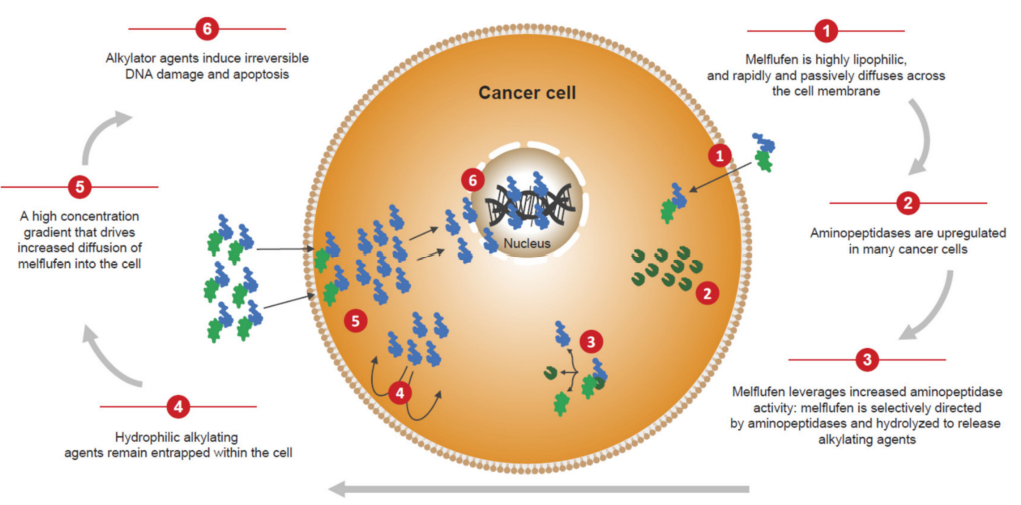
Melfulfen is a highly lipophilic PDC that utilizes increased aminopeptidase activity to selectively increase the release and concentration of cytotoxic alkylating agents within tumor cells and is currently used in the treatment of multiple myeloma. Another approved PDC is 177Lu dotatate, a form of targeted radiation therapy that combines somatostatin analogues and radionuclides, which is approved for the treatment of gastrointestinal, pancreatic neuroendocrine tumors.
Structure of conjugated drugs
Conjugate drugs developed for targeted delivery typically consist of three components, all of which contribute to the overall biological efficacy and selectivity of the drug. The vector moiety is included in this structure, which targets tumor-specific markers. In addition to peptides, a range of other small molecules and biologics such as native proteins, antibodies, adhesions, engineered ankyrin repeaters, and aptamers have been studied to provide tumor selectivity.
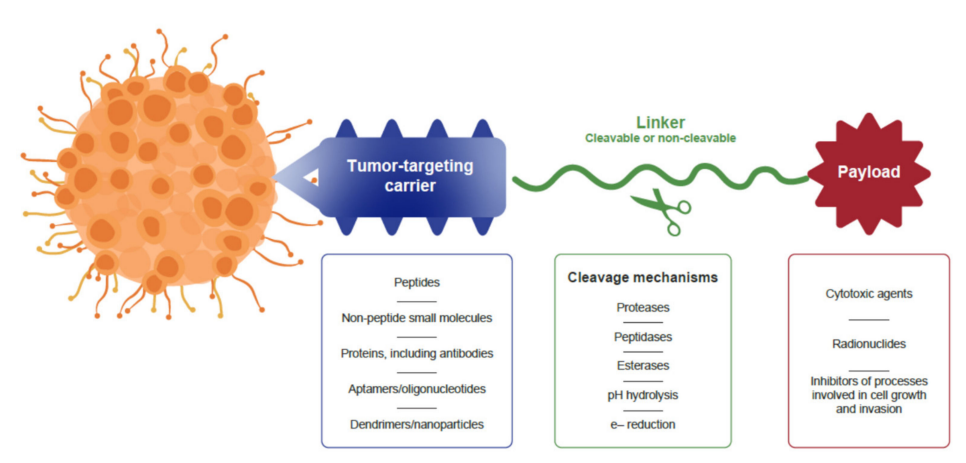
Carrier molecules are linked to active anticancer drugs and can induce a variety of biological functions. Currently, drug conjugates for cancer treatment mainly include cytotoxic molecules and radionuclides that mediate cytotoxicity. Covalent linkers linking targeted vector molecules to effector molecules can be cleavage or non-cleavage. Once the conjugate drug binds to the tumor cell and enters the tumor cell, the cleavage linker is able to control the drug release of the payload. The choice of cleavage or non-cleavage linker depends on the design and mechanism of action of the targeted therapy.
Peptide conjugates for targeted cancer therapy
PDCs have a similar structure to ADCs, but use peptide moieties to preferentially target drug conjugates to tumor cells and limit non-targeted cytotoxicity by releasing cytotoxic payloads at the tumor site or within the tumor.
The use of peptides as carrier molecules in drug conjugates has many benefits; Compared to ADCs, they are easy to synthesize and provide clear and cost-effective targeted therapies. Structural modifications can be easily introduced to support sound drug design to improve bioavailability, binding affinity, and stability. The incorporation of lipids/fatty acids enhances the lipophilicity of the peptide, allowing for adjustment of half-life and bioavailability by regulating tumor penetration and cellular uptake. Peptides are also suitable for combination drug discovery and support in vitro high-throughput screening of candidate structures in order to identify peptides with optimal pharmacodynamic properties. In addition, peptides have low intrinsic immunogenicity.
The peptides used in PDCs fall into two categories: cell-penetrating peptides (CPPs) and cell-targeted peptides (CTPs). PDCs with penetrating cell homing peptides enter cells via non-specific mechanisms, while PDCs with cell-targeted peptides enter tumor cells by specifically binding to antigens or receptors on the surface of tumor cells to mediate cytotoxic payload entry. The application of CPPs is limited by their low cell specificity. In contrast, CTP exhibits similar effects to monoclonal antibodies while overcoming some of the shortcomings of monoclonal antibodies, so it is widely used.
Melflufen is a highly lipophilic PDC that quickly and passively crosses cell membranes. Once inside the tumor cells, Melflufen's aminopeptidase-binding domain is acted upon by aminopeptidase and esterase and releases the payload of the alkylating agent. A series of aminopeptidases expressed in multiple myeloma and other tumors mediate hydrolytic lysis and rapid release of cytotoxic payloads from Melflufen, triggering DNA breaks, intrastrand, and interstranded DNA crosslinking by modifying DNA, preventing cell division and leading to cell death.
177Lu-dotatate is a targeted form of radiotherapy that combines somatostatin analogues and radionuclides, linked by the chelating agent DOTA. Somatostatin receptors are expressed in more than 80% of well-differentiated neuroendocrine tumors, which provides an ideal target for PDCs that use somatostatin analogues as homing peptides.
Clinical application of PDC in cancer
Only two PDCs are currently approved by the FDA for clinical cancer treatment: Melflufen and 177Lu-dotatate.
Melflufen in combination with dexamethasone is approved for the treatment of patients with severe relapsed or refractory multiple myeloma (R/R MM). The FDA's accelerated approval of Melflufen is based on the results of the Phase II HORIZON study, which targeted patients with severe treatment, drug resistance, and high-risk RRMM. Melflufen had an overall response rate (ORR) of 29% in the overall population and 26% in patients with tertiary refractory MM. Melfulfen is effective in refractory MM patients with multidrug-resistant, high-risk cytogenetics, and/or extramedullary disease. In addition, the results of the Phase III OCEAN study (NCT03151811) showed that Melflufen plus dexamethasone had a longer progression-free survival (PFS) in patients with RRMM compared to standard treatment with pomalidomide plus dexamethasone. Recently, however, Melflufen was withdrawn for safety reasons.
The approval of 177Lu-dotatate is based on the results of the Phase III NETTER-1 study, which showed that giving 177 Lu-dotatate once every 8 weeks (for a total dose of four) in combination with octreotide (LAR) every 8 weeks had significant advantages over LAR alone in terms of PFS, ORR, and OS.
Two PDCs currently in clinical development target the Sortilin1 (SORT1) receptor: TH1902 and TH1904. The SORT1 receptor is overexpressed in several malignancies, including breast and ovarian cancer. TH1902, a PDC with a docetaxel payload, received fast-track designation from the FDA for the treatment of patients with sortilin-positive recurrent advanced solid tumors that do not respond to standard treatments. TH1902 is currently being studied in Phase I clinical trials and TH1904 contains a doxorubicin payload and is currently undergoing preclinical studies.
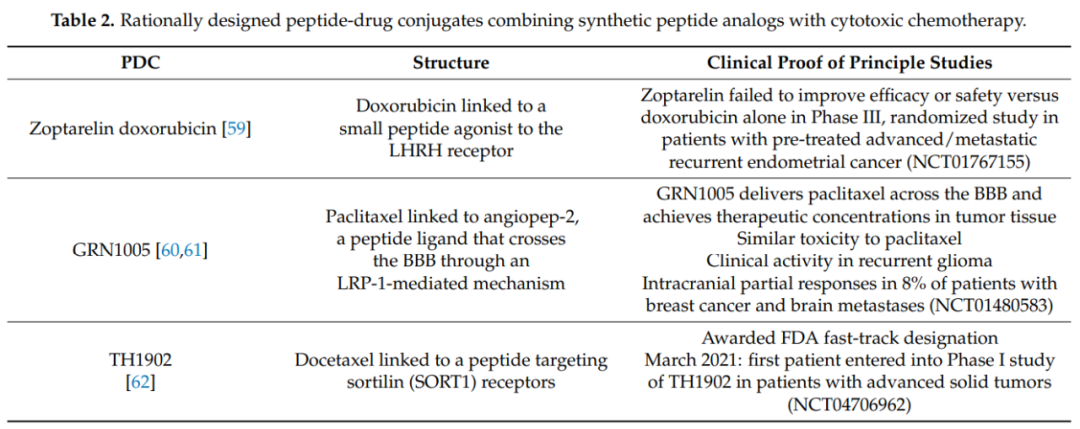
Other PDCs in clinical development include synthetic analogues of natural peptide ligands linked to cytotoxic chemotherapy drugs, including doxorubicin and paclitaxel. So far, the results of these PDCs have been mixed, suggesting that there are still some challenges in translating the good pharmacodynamic properties of PDCs into improved patient outcomes.
The future direction of PDC
With the application of new technologies that support the development of new PDC models, peptide conjugate drugs will continue to advance as a new frontier for the treatment of cancer.
Affibodies (consisting of 58 amino acids) and albumin-binding domain-derived affinity proteins (ADAPTs; Composed of 46 amino acids) are two classes of polypeptides that fold into stable trihelix bundle structures and can be designed to bind selectively with high affinity to a variety of target structures, including cell surface receptors on tumor cells. These peptides are very promising for use as targeting units in future PDCs, particularly due to their typical high affinity, ease of production, and control of drug molecular loading and spatial arrangement.
Bicycle-toxin conjugates (BTC) is another new form. The tumor homing fraction is a synthetic bicycle peptide (9–20 amino acids) consisting of three cysteine residues. As with other PDCs, the advantages of BTC over ADCs include enhanced tumor penetration, rapid extravasation, and slower renal clearance. Many BTCs are in early clinical development, and BT5528 contains a bicyclic peptide that targets the tumor antigen EphA2 via a cleavetable linker linker to MMAE. A Phase I/II study (NCT04180371) in patients with recurrent advanced solid tumors expressing EphA2 is ongoing.
Dendritic peptide complexes are another promising drug delivery modality. Dendritic macromolecules are nanoparticles that can envelop cytotoxic drugs, and they are composed of spherical molecules made up of branching layers. The use of functional groups or peptide sequences to modify the surface of dendritic macromolecules to target receptors or other cell surface antigens can be used to create "smart nanoparticles" that target cancer cells.
Self-assembled PDCs are an emerging subset of PDCs in which conjugates are able to form nanostructures with unique physicochemical properties. Thus, the drug delivery vehicle formed by self-assembling PDCs has the ability to break down over time or due to specific stimuli in order to release the active drug. Self-assembling PDCs help avoid premature degradation and rapid clearance of active drugs. For example, camptothecin and paclitaxel-based self-assembled PDCs have high drug loads and excellent stability. Self-assembled PDCs can enhance the accumulation of active drugs at the tumor site by enhancing permeability and retention effects.
Brief summary
PDC as a novel treatment has the potential to overcome some of the limitations of ADCs, however the recent withdrawal of melflufen shows that there are still many challenges in the clinical application of PDC. With more innovative methods being studied, it is expected that safer and more effective tumor-targeted PDCs will emerge, bringing hope to patients with refractory cancers.
Article from: Health Community

 Contact Us
Contact Us
 Return
Return